An overview of IUI
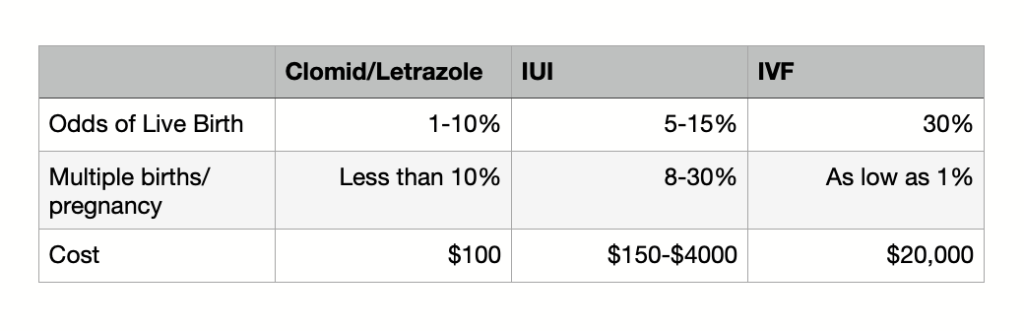
If you have already tried clomid or letrazole for a few cycles with no result, your provider will likely recommend an IUI. It’s important to remember that an IUI is a little more effective than taking clomid or letrazole, but significantly less effective than IVF. For some patients, IUI may work, but for others it has no chance of working. IUI can work for patients with PCOS or ovulatory issues, a single blocked tube, lesbian couples or single women, unexplained infertility and potentially male factor infertility. It is of little to no use for women with low egg supply, two blocked tubes or uterine issues like scar tissues or a septum, or severe male factor infertility.
If IUI is going to work, it will work within three to four attempts. After that, data shows that the chance of getting pregnant is very low. IUI does raise the risk of multiples.
Important decisions for an IUI cycle
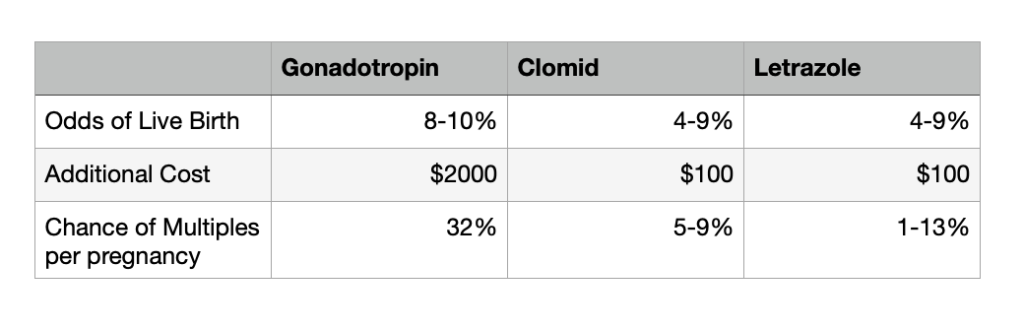
There are several decisions for you and your doctor to make: choice of medication, whether or not to do monitoring, whether to ovulate naturally or use a trigger shot, and potentially whether to use fresh or frozen sperm. Clomid and letrazole have similar efficacy, though letrazole may be a better choice for women with PCOS. Gonadotropins are significantly more expensive and require monitoring because they greatly increase the risk of multiples.
Monitoring verifies that at least one follicle is growing and helps ensure that ovulation and insemination match up. However, it costs more and requires additional appointments.
There is no data that using a trigger shot improves birth rates, however it does help your doctor time the IUI. For patients who find OPK testing stressful, it can be helpful to do monitoring and a trigger shot. Gonadotropins require a trigger shot.
Generally, cycles with fresh sperm are two times as likely to work.
Looking at effectiveness of IUI by patient type
In general, the effectiveness of IUI depends most on your age, the type of medication you are using, and the number of follicles produced.
Unexplained Infertility – Success rate is 5-10% per cycle versus 40-50% per IVF cycle. After three unsuccessful IUI cycles, the success rate decreases.
PCOS and Ovulation Disorders – IUI can be helpful for this group, depending on the sub-type. If the issue is hypothalamic dysfunction with FSH and LH near zero, you will need to use gonadotropins. If you have PCOS or “PCOS-like” signs with no period or an irregular period, medicated cycles can be very helpful. Letrazole appears to be a better choice for women in this group, particularly if your BMI is above 30. Adding IUI to a medicated cycle can be helpful if there is a mild male factor or if medication has produced an ovulation but no pregnancy after timed intercourse, though some studies have shown that adding IUI for this subgroup of women does not improve pregnancy rates. Gonadotropins can greatly increase pregnancy rates in this group, but also the risk of multiples. If you’re thinking of moving to gonadotropins, it is worth your time to get a second or third opinion.
Blocked Tube – IUI can work when one tube is blocked, but not if both tubes are blocked. Success rate depends on where the blockage occurs. If the blockage is near where the tube meets the uterus, there is a 38% success rate after three IUI attempts. If the blockage is near where the tube meets the ovary, the success rate is 12% after 3 IUI attempts. This is because HSG tests are wrong 30% of the time, and they are most often wrong about blockages near the uterus. If the HSG says you have a blockage near where the tube and uterus meet, you may not, in which case your chances are good with IUI.
Male Factor – Success rates depend on the man’s total motile count. There is disagreement on whether IUI is an appropriate for men with a total motile count of less than 10 million. Keep in mind that a sperm wash can lower total motile count by roughly a third. Record you pre and post-wash total motile count to see how much a wash impacts your count, and keep this in mind when deciding whether to do a subsequent IUI.
Risks of IUI
Clomid is an anti-estrogen, which prompts the brain to produce more LH and FSH. In a subset of women, the uterus responds by thinning the lining. This can be cumulative, getting worse with each cycle. Hot flashes and mood swings are fairly common with clomid. There is an increased risk of multiples, though the level of risk depends on the medication you are using. There is also a risk of ovarian hyperstimulation, but even with gonadotropins that risk is very low.
When to start IUI, and when to move onto something else
When a woman starts with IVF or quits IUI very quickly, she ultimately gets to a baby faster than a woman who starts with IUI or sticks with IUI for a long time. Important factors to consider are your age, your desired family size, your underlying diagnosis and the duration of your infertility. Cost is also a factor—IVF is expensive. Don’t feel guilty if cost is one of the factors you are considering.
IUI can be effective for women. The problem I’ve seen in my practice is when a woman sticks with IUI for such a long time that she ends up spending as much money on IUIs as she would have on an IVF cycle. The odds between the two procedures are significantly different. It’s better to look at both procedures up front so you can create some guidelines with your partner about the decisions you want to make. An ob/gyn will often push IUI because that is what he/she is able to offer you. An RE will often push IVF because that is what he/she is able to offer you. Keep that in mind as you make your decisions.
Questions?
I’m here to help. Feel free to give me a call at 920.574.0447 or send me an email at leah@leaholson
***Data in the above tables is from fertilityiq.com
