What are my odds?
There are two major determinants of IVF success: a woman’s age and her clinic. A patient’s underlying condition (e.g. endometriosis, PCOS, male factor) plays a role in the odds of success, but probably less than you’d guess with a few exceptions: diminished ovarian reserve, severe male factor, true uterine factor, and recurrent pregnancy loss.
It’s important to remember that although success closely correlates with age, even women under the age of 35 have odds of less than half from one cycle. Most women will go through multiple cycles before delivering a child. The first IVF cycle is the most likely to work, with each subsequent cycle slightly less likely to work. In women under 38, IVF success rates are three to five times higher than IUI, but cost five to forty times as much.
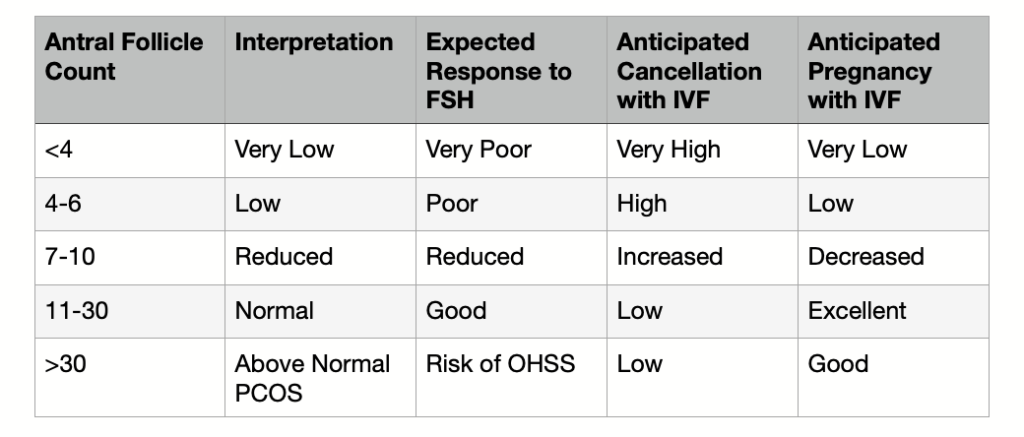
Antral Follicle Count and IVF Predictions
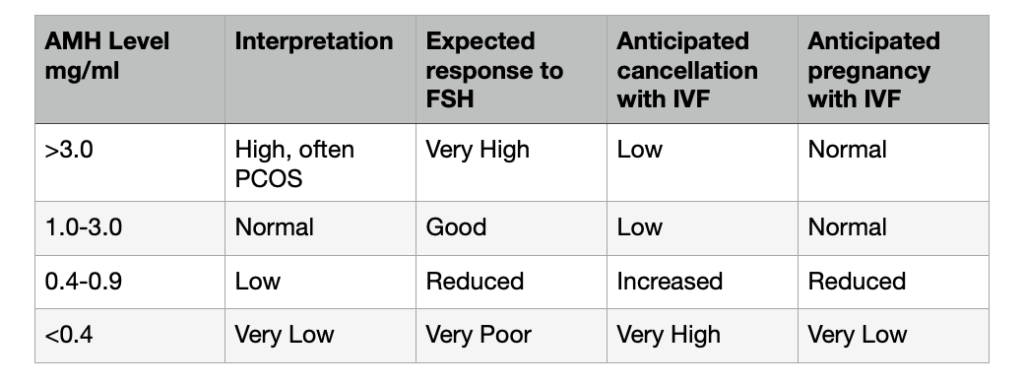
AMH Levels and IVF Predictions
To get an estimate of your odds, check out https://www.cdc.gov/art/ivf-success-estimator/index.html
The importance of the IVF Lab
Growing embryos is the most difficult part of the IVF process. A good IVF clinic can increase your chances of success twofold during any given cycle. The IVF lab is a significant component in the overall quality of the clinic. The IVF lab has a number of important tasks: to fertilize as many eggs as possible, to cultivate resulting embryos to a healthy state, to be able to biopsy the healthiest embryos for genetic testing if required, and to freeze or thaw either eggs or embryos for future use. Each one of these tasks can be measured so that you can compare labs.
The following suggestions are based on a survey of twenty embryologists done by fertilityiq.com. Evaluating labs is complicated because results depend in part on the mix of patients that a specific clinic sees. In order to resolve this issue, the best thing is to compare the success of egg donors. Look at these key performance indicators: fertilization rate, blastocyst conversion rate, successful PGS biopsy rate, blastocyst cryosurvival rate, results like implantation rate.
Fertilization: A passable lab should fertilize a minimum of 60-65% of retrieved eggs. A benchmark lab should have fertilization rates into the high 70s or low 80s.
Blastocyst Cryosurvival Rate: Many IVF cycles have at least one embryo to freeze. Passable lab will have 90% of embryos survive after thawing. A benchmark lab is closer to 99%.
Implantation rate: Embryos from a passable lab should implant 30% of the time. Benchmark labs should be at 60%.
There are a few other things to consider. Ask if your clinic has a disaster recovery plan in place. I had one patient whose cycle was cancelled at the last minute due to flooding. Make sure the lab is open seven days a week.
Comparing Clinics—A Cheat Sheet
To find statistics for your IVF clinic:
- Go to the CDC.gov website and search “assisted reproductive technology:
- Click on Latest ART Success Rate Clinic Reports, but keep in mind the current data is 2-3 years behind
- Select a state on the map to look a individual clinics within the state
- Select a specific clinic and click on the Detailed Data Summary tab
Important Things When Comparing Clinics:
- How many cycles are they doing for each age group? Smaller groups mean less reliable statistics.
- What are their stats in your age group? The most basic things to look for are:
- Outcomes per cycle (percentage of cycles resulting in live births)
- Outcomes per transfer (percentage of cycles resulting in live births)
- Frozen Embryos from non-donor eggs (percentage of transfers resulting in live births)
- How to choose between clinics?
- If success rates are similar, the labs and skill of technicians is probably similar. Make your choice on cost, location, etc.
- If there are large differences in success rates, this likely indicates differences in labs.
- If you’re in an older age group and the stats are low across the board (this is common at a higher age range) check the success rates for donor cycles or younger age groups. This will help you see if there is a lab/skill difference from clinic to clinic.
What is my protocol?
There are two main protocols: the long agonist protocol or the antagonist protocol. Both cycles have the same results, but the antagonist cycle can eliminate the risk of OHSS. A flare cycle can be used for low responders, but it is not as frequently used as it used to be. Low dose seems to be more successful, or combining oral agents with injectables.
Poor responders or women with low ovarian reserve will not get many eggs no matter what, and research shows using a low dose gets as many eggs as a high dose. That can save money and might benefit egg quality. If the follicle count is a bit higher, say 6, and the woman only gets 3 eggs, it might make sense to change up the protocol.
Should I do a frozen or fresh transfer?
Both types of transfers have advantages, but overall there are more advantages to freezing all embryos and then doing the transfer at a later date. There is a short window of time during which a uterus is most receptive to absorb an embryo and the embryo is most ready to implant. During a fresh cycle, levels of estrogen and progesterone may be ten times higher than normal. This can pull forward the uterus’s “window of receptivity”, which may close before the embryos are mature enough to implant. For this reason, success rates tend to be higher in frozen cycles.
There are additional factors that might make a frozen cycle more appropriate: if there is a high level of progesterone at retrieval or the uterine lining doesn’t look optimal, if the woman might have endometriosis, women with PCOS, Asian or African-American women, women who want to do genetic screening, and women who are at risk for OHSS.
There are some reasons to prefer a fresh cycle. Fresh cycles are less costly and have a faster time to pregnancy.
What is ICSI and is it necessary?
It is important to remember that up to forty percent of eggs can’t be fertilized. There are two methods to choose from for insemination, but most clinics use just one technique on all their patients regardless of whether it is appropriate. Conventional insemination is used in a third of cases, and comes closest to recreating the “best sperm wins” conditions of natural insemination.
ICSI (Intracytoplasmic Sperm Injection) is used in two thirds of cases. The embryologist uses their judgment to select the best sperm and then injects it into the cell. Experts will say they are not as good at choosing sperm as they would like, with some even calling the selection method “haphazard”. For most patients, ICSI has no impact on the odds of whether their cycle will work. It will result in more eggs being fertilized, but that rarely translates into a higher birth rate.
For women who produce less than three eggs on their prior cycle, conventional insemination actually leads to higher birth rates. For men with severe male factor infertility, ICSI gets much better outcomes. ICSI also results in better live birth rates for patients who had fewer than twenty percent of their eggs fertilize in a previous cycle.
Should I do genetic screening?
Pre-implantation Genetic Screening (PGS) helps avoid transfers of embryos that are unlikely to lead to pregnancy and live birth. Particularly in older women, it cuts down on the likelihood that a transfer will fail or end in miscarriage. It also helps promote single embryo transfer. On the negative side, it costs around $5000 and does nothing to increase the odds that an IVF cycle will work. Some doctors fear that the test’s inaccuracies could confuse a good embryo for a bad embryo. There is data that shows similar patients who had their PGS biopsies run at different reference laboratories got back very different results.
Consider insisting that “mosaic embryos” are broken out as a separate category. They are often put together with aneuploid embryos, which have much worse prospects than mosaic embryos.
The decision on which embryo to transfer is made using the following criteria: how fast the embryo is developing, morphological grading, and PGS. The speed at which an embryo reaches any given stage correlates with its odds of success. An embryo that has better morphological traits is more likely to lead to a live birth than an embryo with poor morphological traits. However, morphology is not predictive of whether an embryo will lead to a healthy baby or not. Great looking embryos often fail and less good looking embryos often work.
This is one of those hard decisions in IVF where there are no right answers. Discuss the pros and cons with your provider and partner. Whatever decision you make, it is the right one for you and your particular situation.
How much will this cost? Should I do a shared risk program?
The average fertility patient undergoes over two cycles, so the cumulative IVF costs for most patients is between $40,000 and $60,000. There are financing options available, typically as loans with annual rates similar to those offered for other types of medical services.
Half of US clinics offer patients a package discount or have a refund feature. The authors of FertilityIQ.com have mixed opinions on the programs, but typically believe that they are offered to patients who are likely to succeed early in treatment. Two thirds of refund patients succeeded in the first cycle. Thus, customers often dramatically overpay for results they would have achieved. Plus, the list of exclusions if often quite large (e.g. medication, genetic testing, pre-treatment testing). Most patients spend 20-50% beyond the quoted price.
For more in-depth analysis, check out www.fertilityiq.com/cost/ivf-refund-and-package-programs
Questions?
I’m here to help. Feel free to give me a call at 920.574.0447 or send me an email at leah@leaholson
***Data in the charts above is from fertilityiq.com
